This activity has expired. Credit is no longer available.
This activity is supported by educational grants from AbbVie Inc. and Celgene Corporation.
Enhancing Shared Decision Making in Relapsed/Refractory Multiple Myeloma (RRMM)
Sandra Kurtin, PhD, ANP-C, AOCN®
The University of Arizona Cancer Center, Tucson, Arizona
Kevin Brigle, PhD, ANP
Viginia Commonwealth University Massey Cancer Center, Richmond, Virginia
Josh Epworth, MSN, ARNP
University of Washington, Seattle, Washington
Learn how to incorporate patient-centered communication and shared decision making in your practice, thereby improving patient and caregiver adherence, satisfaction, and engagement.
|
|
|
|
|
|
Transcript
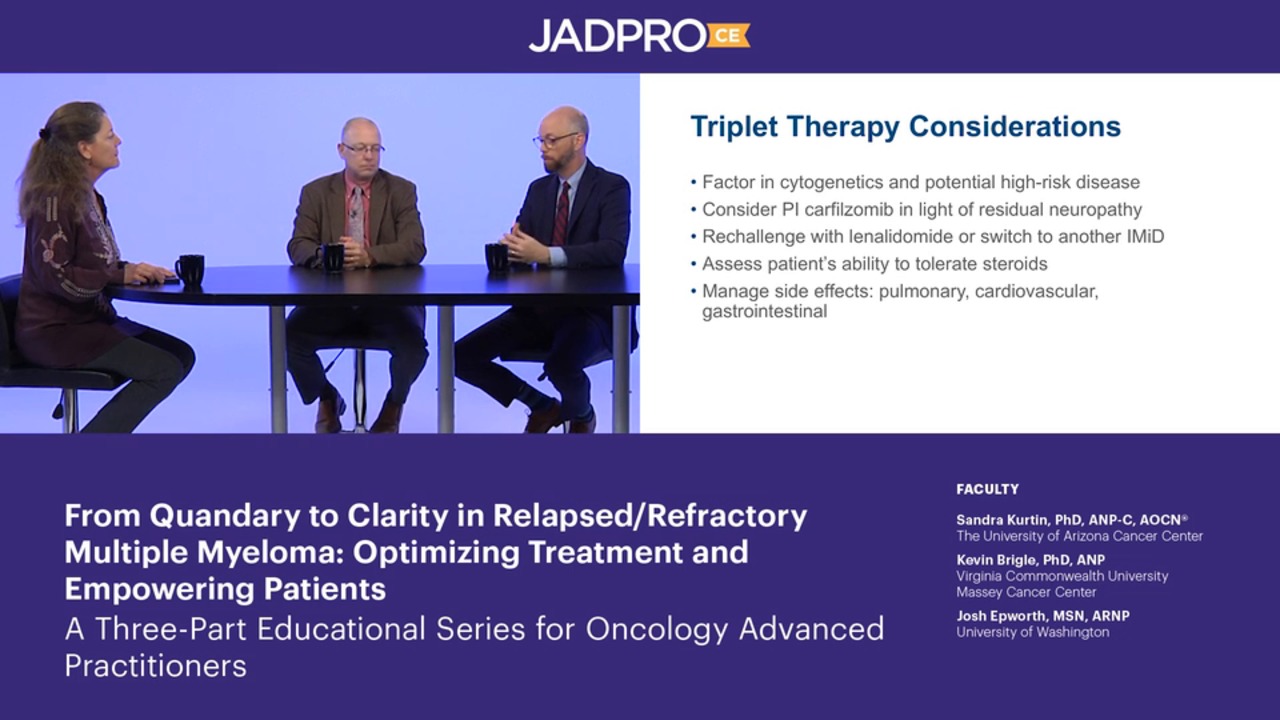
Sandy Kurtin: Hello, and welcome to "From Quandary to Clarity in Relapsed/Refractory Multiple Myeloma: Optimizing Treatment and Empowering Patients”—a 3-part educational series for oncology advanced practitioners. I'm Sandy Kurtin, nurse practitioner at the University of Arizona Cancer Center. And I'm joined by my 2 colleagues.
Kevin Brigle: Hi, I'm Kevin Brigle. I'm a nurse practitioner in the hematologic malignancies clinic at the Massey Cancer Center at Virginia Commonwealth University.
Josh Epworth: Hi, I'm Josh Epworth. I'm a nurse practitioner in hematologic malignancies at the University of Washington, Seattle Cancer Care Alliance in Seattle, Washington.
Sandy: In this video we'll be discussing the important role of shared decision making in the treatment process for relapsed/refractory multiple myeloma.
Sandy: Let's talk a little bit about shared decision making as a model, or a process really, in multiple myeloma, specifically in relapsed/refractory multiple myeloma. So we know that this is a process that involves clinicians, patients, and caregivers really working together to help make decisions, and we know that it's particularly important to patient and caregiver engagement in that process. We understand that it plays a role in people being adherent to their treatment plan, and we know that it's been correlated with patient and caregiver satisfaction, so they're feeling like they're part of making decisions about their health, but there are several fundamental tenets and that means that the patient is informed about the decision, meaning that we have to have clinicians capable of providing the necessary data and information for those patients to make those decisions, that there's a decision to be made, that we're informing them about risks and benefits of treatment, and we know that they're able to understand what we're saying, and what kind of modality, and so we use a lot of tools or other strategies; we're going to talk about those using some cases in a moment. But I think we also make the assumption that clinicians understand patient-centered communication and how best to communicate very complicated data, which we've talked about in the previous modules in this series, to a patient and their caregiver so they can make those kinds of decisions.
Sandy: So one of the tools that is out there is called the SHARE model—SHARE standing for S, Seek your patient's participation; H, help your patient explore and compare treatment options; A, assess your patients values and preferences; R, reach a decision with the patient; and E, evaluate your patient's decision.
Sandy: We know that we primarily talk about shared decision making when we're really talking about treatment decision making, and that's particularly important where we have more than 1 reasonable option. And we've talked in previous modules about the difficulty we have in the relapsed/refractory setting. With sequencing and knowing that there often are more than 1 option, where no 1 clear option has an advantage. So we know there are good drugs, good combinations of drugs, and sometimes that's tailoring that to the individual patient and balancing that risk and benefit. There are a number of websites and strategies and tools that I know I use in my practice and have the patients referred to or the advanced practitioners. For advanced practitioners, certainly we refer them to the APSHO website, the journal JADPRO. We know that ASCO sponsors Cancer.Net, which is geared toward patient information, the International Myeloma Foundation, and the Myeloma Research Foundation are great tools for both advanced practitioners and patients. So, we're going to use a couple of cases to talk more about how you would apply all of this in using shared decision making and patient-centered communication with specific types of patients.
Sandy: So the first case is a 66-year-old female. She has relapsed/refractory multiple myeloma, started assessed stage II, IgG lambda, multiple myeloma. FISH revealed a gain of 1q and a translocation of (4;14). Now, she's a very busy CEO, she travels internationally, so is always on the go. She also splits her time between her residence in the East Coast and the West Coast, which is not unusual in my state of Arizona, where we have a lot of retirees, and they come in the winter, and they go back home to where they live in the summer. She was treated with a very standard 3-drug regimen, immunomodulatory agent, proteasome inhibitor, and dexamethasone but declined to have an auto transplant, and that was primarily due to her busy lifestyle and she felt like that she could just not dedicate the time to transplant. So, unfortunately, after 7 months of a treatment break, we see her moving up in her serum free light chains and M protein. So, she's ultimately now relapsed, but still declining an auto transplant because she's still working. So this is a difficult situation where sometimes what we might have recommended to a patient they choose not to do.
Sandy: So Josh, can you talk about how you would approach this case using the paradigm of patient-centered communication and shared decision making?
Josh: Sure. You're right. She is in a significant, difficult position. She has a very aggressive-appearing disease, but also a series of lifestyle desires that don't allow us to take the aggressive stance that we would typically like. I would open up the conversation with – and one of the things I would like to put in is that our patients are infinitely better informed now through the resources that you brought up than they have been in the past, so we have to be aware that they've been doing some reading and are already coming in with some thoughts of what they like. But I think the first thing is to find out what are her expectations of what we can do. And then once we have that understanding, start having some conversations about what we can do for her based off of is it an all-oral regimen that she's wanting? Is it an aggressive regimen that is broken between 2 facilities? I'd really like to ask her some questions about what does she expect, what is she willing to do, and what does she expect the outcome to be.
Sandy: Great, and, Kevin, how would you bring in other members of the interdisciplinary team, and what other tools might you use in your practice in this situation for this patient?
Kevin: Yeah, I think the challenge here is that you pointed out she's getting the information from 2 sides of the country. Where we are in Virginia, it's very often, north/south we get situations like that. And so, I think for starters, even to say, well, what have they told you there? And what do we know here, so we're all on the same page to begin with, in terms of potential treatment options. And then I think the other thing we would need to look at, and Josh pointed out, that whatever we choose may not be what she would choose, and so she's looking at immediate things and one of the things I think we would look at too on this patient is what are your long-term goals? Because the choice you make now may not make those very tenable. And so I think that's the big thing right there. But again, we use every member of the, basically, our care team as needed. I'm not sure what she needs right now other than just information, strong information, again, that information which says, "Well here's your long-term goals. And how do we meet those?”
Sandy: Well, we talked a little bit about some of the online resources that are available. Are there others that you use, Josh, in your practice for the multiple myeloma population where they might get information perhaps from another patient?
Josh: Well, there's a great one. I like to use the Myeloma Beacon for a host of reasons. One, it's a good layout, it is reasonable in its approach, it's got providers who specialize in multiple myeloma who make commentary on it. So the statements that are made on it are a little more reliable than I've seen in other places. And as far as official areas, I really like mSMART from the Mayo clinic simply because the language is patient-centric and it is one of the great facilities in treating this disease, and they are oftentimes coming up with the best new information, which patients are always seeking at this point.
Sandy: And I know, Kevin, you're involved with International Myeloma Foundation. Talk to me a little bit about some of those resources and patient-centric meetings that they have to help in this situation.
Kevin: Right. And so the International Myeloma Foundation and the Nurse Leadership Board puts out a number of important publications, which are directed toward patients. The International Myeloma Foundation has a lot of understanding series as well in terms of a lot of different drugs and things like that. And the other thing the International Myeloma Foundation does is they support all the area support groups, and I forget the exact number of them now, but there's any number of support groups in states and beyond going to the web and getting some good information from different patients. You cannot beat what happens at those support groups as well.
Sandy: Just having that conversation about what might you do and what did I do and what was the outcome really being able to see that.
Kevin: Absolutely. One on one. Right. And sometimes seeing someone who's gone through what you're afraid of and is doing very well, it can be very powerful.
Sandy: Great, that's great. So let's talk a little bit, we talked a little bit about patients whose decision might not be what we would decide, which is always a challenge, but we know there are a number of barriers to patient-centered communication and shared decision making and there was an important recent publication talking about this across all hematological malignancies, and they categorize this into clinician-associated, patient-associated, and infrastructure- or facility-associated. And we know the facility-associated infrastructure, a lot of that is time because these conversations do take time. We've mentioned a few patient examples and then we know there are others for clinicians in terms of just information exchange and then specifically treatment decision making. So talk to me a little bit about, in your practice, what are the barriers that you see and then also I want to talk a little bit about the struggle for having consistency of message across clinicians. So, Kevin, let's start with you.
Kevin: Right? So I think when you look at that group, it is divided into patient and provider and institution, but I think some of the things we have to look at too is dividing that a little bit differently, into, what are modifiable things, what can we change, and what can't we change? And you'll see on that group, there are things like cultural and religious. Well, clearly we're not going to be able to change those things, but we should be able to work with those things. So, things that might be financial or transportation, those are the things we can probably work on. And that's where, again, bringing in the whole patient team is really important. And so that's also the importance of the tumor board where we have the social workers, and we have supportive care, and we have all the different disciplines there to help with these particular cases that are going to be really, really difficult.
Sandy: So we may have the regimen that we feel is best for that patient but logistically may not be feasible for that patient, and therefore they choose not to pursue that because of the things that you've talked about.
Kevin: Correct, so how do we overcome those challenges to give them the regimen that we think is best?
Sandy: Great, and, Josh, tell me a little bit about your approach and how do you try to create this consistency of message in your practice, so within at least in your own institution your message is more the same than different for patients.
Josh: What we really look at, is, – we start with consistency of message in our own team. And things modify constantly. And so it's very important, as the advanced practice provider working with an MD, is that you are communicating frequently so that when if an email comes in to both of you, it's very easy to give a response that is slightly different than what you're attending would do, the attending that you're working with would do, and that can create some anxiety for the patient. So I think making sure that you're meeting with the attending or the other physicians that you're working with or the other APs and making sure you're onboard the same page. That's just in the team, and then when we're talking about an institutionalized issue – the facility I work with in the state, it has significant divide between urban and rural and a lot of our patients are over 65 coming in a great distance to come into the middle of the city and receive treatment, which can be very difficult for them.
Josh: So it brings up the question, can we reach out to satellite facilities? Can we utilize these groups and communicate closely with them so that we're acting as more a consultancy group and they're acting as the administrative group?
Sandy: So really co-managing these patients, but being sure that you're providing them with adequate information so that there's continuity across the settings.
Josh: Exactly. And the last part I view is that in the state I work in, there are multiple language groups, and we really want to make sure that we are utilizing official interpreters as opposed to family members, that can create some friction in certain cultures, and it also can create misunderstanding, and so we really reach out and say, let's make sure we're using the right person to do the speaking between us.
Sandy: So that's really great information. So let's talk a little bit now about when you're talking about outside institutions. I'm going to share a case with you now. This is a 77-year-old female kappa light chain disease diagnosed in 2015 relatively refractory disease, high risk. She basically has had multiple prior therapies in all of the different classes, lenalidomide, bortezomib, dexamethasone, ixazomib being an oral proteasome inhibitor moving on to daratumumab as an anti-CD38 antibody and was actually primary refractory to that antibody really emphasizing that there are those patients who do not respond to these newer agents. And so she's now been through really all available FDA-approved therapy. She's 80 years old and her husband has Alzheimer's and she feels like she needs to keep going and is very motivated and wants to seek out what's next. So this is a difficult situation. She has good family support in her daughters. But talk about how you might work with this patient who's 80 who's had a lot of therapy, but is otherwise in pretty good shape and highly motivated, Kevin?
Kevin: Yeah, these are going be more and more challenging cases. And so I think the key here is she's very motivated, so she doesn't want to stop therapy and she wants to stay basically around to take care of her husband. And so to try and honor that, we probably need to find something to treat her with, but at 80 years old do so in a way that's going to not make her nonfunctional so that she can do that, and that becomes more of a challenge as you said; she’s been pretty much through everything. And so perhaps we can also reach into our bag and grab some older drugs such as cyclophosphamide, which is fairly well tolerated but does have some side effects and can maybe potentially keep herself functional, and bring these up to her.
Kevin: I think the important thing here is too is that we are running out and she has gone through many of these regiments very quickly. And if we've done our part, we've done some shared decision making all the way through, and along that pathway have said, "Look, you're going through these things and at some point we're going to be running out of the medications that we can use." And so, you've already set her up for that time that that's going to happen, and the family as well. And so hopefully, they're making some changes, some family choices as well to help with that.
Sandy: So talk a little bit more, Josh, if you will, about how do you integrate your interdisciplinary team in helping people through these multiple transitions of care and bringing up and reminding people about palliative care and supportive care and ultimately that this remains an incurable disease.
Josh: Well, the palliative question is a great one, because there is a very common misconception that palliative equals hospice, and that's partly our doing by not integrating palliative early enough, that we have the opportunity to really integrate this team early on. So as Kevin was mentioning, these are not new and frightening groups that are being brought in, these are not new and frightening conversations. This is a reiteration of a conversation we've had multiple times. But I think one of the questions to ask with this patient, and it kind of goes back to your question, is why does she have to do this? What are her expectations? Can we have a conversation where she can have confidence that her husband will be well taken care of if she's not there? Because as Kevin brought up, the medications that we have, like cyclophosphamide are very good medications, but they have significant side effects. And can she actually expect to function at the level that she wants to for her husband and still be able to treat herself? So that would then bring in, do we bring in chaplaincy and have the conversation, if that's relevant to her?
Josh: Really trying to meet her where her personal culture is and make her aware that she has more than just herself to take care of it, and then try to make a determination of if she's bound and determined to be there, try to find his, Kevin mentioned again that, what is the medication that will hold this disease in place as best as possible and have the least impact on her quality of life?
Sandy: I think you bring up a really important component, both of you, is that we really need to understand the patient beyond their disease, we need to understand their support system we need to understand their expectations, and what's driving them. We know there are people that just want to see a grandchild born or a great grandchild a born or somebody graduate from college, or get married. And so, really, what is that motivation for them to continue treatment and really incorporating that interdisciplinary team.
Sandy: So let's shift gears and talk about a much younger patient. So case number 3 is a 59-year-old IgG kappa multiple myeloma, a male, and he's been living with myeloma for 14 years, so he was diagnosed in 2005, he's working full time. He's the primary wage earner in his family. He does have one adult daughter and he's had actually 2 transplants over the course of time, when we used to do tandem transplants back then, and has gone on to have a number of other therapies including immunomodulatory agents, proteasome inhibitors in really early and late development, and also has had the anti-CD38 antibody, daratumumab most recently, but we're starting to see those light chains ticking up.
Sandy: He does not want to have an allogenic stem cell transplant. And we can talk a little bit more about that in general. And his primary concern is a health-related quality of life, and that he would be unable to work after an allo transplant, and he's very concerned about family finances. So talk to me a little bit about this patient and the balance of quality of life and are more aggressive therapies for these patients who are 14 years out and have had multiple lines of therapy, Kevin.
Kevin: Again a tough case. And we understand his motivation. He's had this disease for a long time, we've been treating it, he's been managing, we've been managing to keep him functional and working and he probably assumes he'll be able to do the same again without a transplant. I think the big fear we have when we see someone like this is even though they don't want to go through transplant, that this because they may not be able to work later. This disease may progress and, by the disease itself, make working not an option. And so I think I understanding this whole part and that he needs to work. And so I think it really behooves us to try and find something then that will work with that. We understand his motivation. So is it a clinical trial? That might be the best option that we can get him to them as well—something that doesn't impact his time significantly. But he is definitely going to need some type of novel treatment, and so doing that within the constraints of his working and keeping insurance and things like that are probably the key thing here.
Kevin: And can I just say, get him in contact with our financial people as well for planning.
Sandy: Yes. Absolutely, and Josh, you're in a large center, and you run a lot of clinical trials, but there are a lot of settings where you don't have access to a trial in your own center, and so essentially you're going to have to travel for treatment in these cases where there isn't an available FDA-approved therapy. So tell me a little bit about how you work in your setting with these patients, in terms of shared decision making when it comes to a clinical trial.
Josh: Well, I guess the first thing is to figure out what their expectations are and what he's willing to do, because – as you mentioned we have multiple clinical trials, some of which are highly involved, some of which are not as highly involved. If his expectation is I can miss this day of work and I can come in here at this time, then we can say, Okay, then this trial’s out of this trial, but this still is an option, and then the question is finding out what are his expectations of what we can do with a clinical trial? As you mentioned, he's had this disease for a long period of time. He might have this expectation of, we've pulled him out of trouble before, we can do it again. And if that's the case, we need to have a very frank conversation of the position we're in, and maybe that will help him modify his approach.
Sandy: Great. Thank you both for joining us for this activity.
Sandy: We're now going to talk about some PEARLs or a recap of key points and strategies for practice application. Patient-centered communication is prerequisite to shared decision making. Consistency of message across the entire interdisciplinary team is imperative to effective patient-centered communication and shared decision making in oncology. What can we do? We can participate in continuing education programs or training sessions for communication skills. We can catalog available resources in our practice, both human, digital, and print to support the patient in shared decision making and seek out new resources such as those highlighted in this activity. We can be open to patient decisions that are not what we recommend. And we can advocate for a patient-centered communication and shared decision-making model in our practices by sharing national guidelines and best practice strategies and models.
Sandy: Thank you for joining us.
These activities, certified for CME/CE/CPE credit, are jointly provided by
  |
From Quandary to Clarity in Relapsed/Refractory Multiple Myeloma: Optimizing Treatment and Empowering Patients
Activity 3: Enhancing Shared Decision Making in Relapsed/Refractory Multiple Myeloma (RRMM)
Multiple myeloma (MM), a hematologic malignancy plagued by multiple relapses, has seen notable progress in care that has led to improved survival. Contributing to the progress has been an increased understanding of MM pathogenesis and cytogenetics-based risk stratification and the availability of therapeutics such as immunomodulatory drugs, proteasome inhibitors, and novel targeted therapies. Keeping up with these advances is especially challenging for community-based clinicians for whom MM may represent only a small fraction of their total patient population.
With the continued rapid pace of advances in MM, management of patients with relapsed/ refractory (RR) disease is becoming increasingly complex and requires careful evaluation and interpretation of new and emerging data. To help advanced practitioners (APs) enhance their roles as educators and advocates, strategies for effectively educating patients and engaging them in shared decision making are also needed.
From Quandary to Clarity in Relapsed/Refractory Multiple Myeloma: Optimizing Treatment and Empowering Patients is an educational initiative designed to improve the ability of APs to provide high-quality care for patients with RRMM. This initiative includes:
- 3 expert clinical dialogues (video-based activities) certified for continuing education credit
- Downloadable resources including transcripts and slides for each of the certified activities and links to related guidelines, articles, and websites
- Downloadable patient education materials
Release date: 07/31/2019
Expiration date: 07/31/2020
Estimated time to complete: 30 minutes
Fee: None
This activity is designed to help clinicians achieve specific learning objectives, which reflect the desired results of the education. Participants are encouraged to integrate what they learn from this activity into practice to improve patient care and outcomes.
Jointly provided by
Faculty
Sandra Kurtin, PhD, ANP-C, AOCN®
Kevin Brigle, PhD, ANP
Josh Epworth, MSN, ARNP
Intended Participants
This activity is designed for community-based advanced practitioners (eg, nurse practitioners, advanced practice nurses, physician assistants, oncology pharmacists) who provide care for patients with RRMM. Those practicing in academic and comprehensive cancer centers may also choose to participate.
Learning Objectives
After completing this activity, clinicians should be better able to:
- Formulate plans to provide education and tools regarding management of adverse events to patients with RRMM
- Plan strategies for empowering patients to participate in shared decision making
Continuing Education
Certification
This activity is certified for credit by Annenberg Center for Health Sciences at Eisenhower.
39000 Bob Hope Drive, Dinah Shore Building, Rancho Mirage, CA 92270
Voice: 760-773-4500; Fax: 760-773-4513; E-mail: contactce@annenberg.net
© 2019, Annenberg Center for Health Sciences at Eisenhower. All rights reserved.
Statement of Credit
Participants who successfully complete this activity—which includes submitting a completed pre-test, submitting and scoring at least 70% on the post-test, and submitting a completed evaluation form—will be able to download a statement of credit.
To access the learning assessment and evaluation form, visit https://education.annenberg.net/5741-3
Accreditation and Designation Statements

Physicians. This activity has been planned and implemented in accordance with the accreditation requirements and policies of the Accreditation Council for Continuing Medical Education through the joint providership of the Annenberg Center for Health Sciences at Eisenhower and Harborside Medical Education. The Annenberg Center is accredited by the ACCME to provide continuing medical education for physicians.
The Annenberg Center for Health Sciences at Eisenhower designates this enduring activity for a maximum of 0.5 AMA PRA Category 1 Credits™. Physicians should claim only the credit commensurate with the extent of their participation in the activity.

Nurses. Annenberg Center for Health Sciences at Eisenhower is accredited as a provider of continuing nursing education by the American Nurses Credentialing Center’s Commission on Accreditation.
A maximum of 0.5 contact hour may be earned for successful completion of this activity.
Provider is approved by the California Board of Registered Nursing, Provider No. 13664, for 0.5 contact hour.

Pharmacists.
The Annenberg Center for Health Sciences at Eisenhower is accredited by the Accreditation Council for Pharmacy Education (ACPE) as a provider of continuing pharmacy education. This activity has been assigned ACPE Universal Program #0797-9999-19-064-H01-P. This activity is designated for up to 0.5 contact hour (0.05 CEU) of continuing pharmacy education credit. This is a knowledge-based activity.
Disclosures
Commercial Support
This activity is supported by educational grants from AbbVie Inc. and Celgene Corporation.
Relationships of Faculty and Planners
All individuals in a position to control the content of this activity (eg, planners, faculty, reviewers) must disclose all financial relationships with commercial interests that may have a bearing on its subject matter. The Annenberg Center for Health Sciences at Eisenhower has identified and resolved all conflicts of interest in accordance with its policies and procedures. Participants should assess the impact (if any) of the disclosed information on the educational value of the activity.
Faculty
Sandra Kurtin, PhD, ANP-C, AOCN®, is a consultant for AbbVie, Acceleron, Amgen, Celgene, Genentech, Incyte, Novartis, and Pharmacyclics.
Kevin Brigle, PhD, ANP, is on the speakers bureau for Amgen, AstraZeneca, Celgene, Genentech, Novartis, and Takeda.
Josh Epworth, MSN, ARNP, has nothing to disclose.
Planners and Reviewers
Staff of and consultants for the Annenberg Center for Health Sciences at Eisenhower and Harborside Medical Education have nothing to disclose.
Product Disclosure
This activity may include discussion of agents that have not yet been approved by the U.S. Food and Drug Administration and investigational uses of approved products. Please consult prescribing information and practice guidelines for detail regarding safe and effective use of therapeutic agents.
Disclaimer
The opinions expressed in this activity are those of the faculty and do not represent an endorsement by Annenberg Center for Health Sciences at Eisenhower of any therapeutic agent or approach to diagnosis or patient management.