This activity has expired. Credit is no longer available.
This activity is supported by educational grants from AbbVie Inc. and Celgene Corporation.
Therapy for Relapsed/Refractory Multiple Myeloma (RRMM)—Optimizing Use of Current Options
Sandra Kurtin, PhD, ANP-C, AOCN®
The University of Arizona Cancer Center, Tucson, Arizona
Kevin Brigle, PhD, ANP
Viginia Commonwealth University Massey Cancer Center, Richmond, Virginia
Josh Epworth, MSN, ARNP
University of Washington, Seattle, Washington
Review how to optimize the use of current therapies, including incorporating risk-adapted treatment strategies and keeping up to date with evolving guidelines for evaluating treatment response.
|
|
|
|
|
|
Transcript
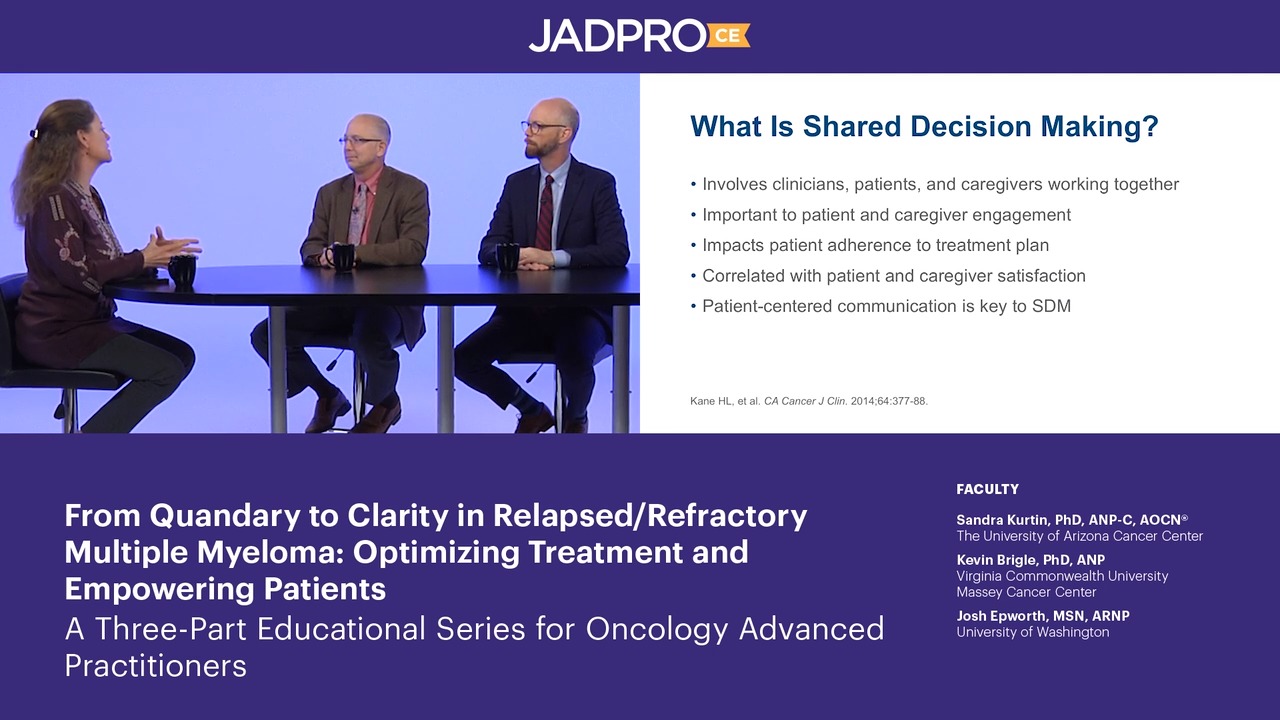
Sandy Kurtin: Hello, and welcome to “From Quandary to Clarity in Relapsed/Refractory Multiple Myeloma: Optimizing Treatment and Empowering Patients”—a 3-part educational series for oncology advanced practitioners. I'm Sandy Kurtin, nurse practitioner at the University of Arizona Cancer Center. And I'm joined by my 2 colleagues.
Kevin Brigle: Hi, I'm Kevin Brigle. I'm a nurse practitioner in the hematologic malignancies clinic at the Massey Cancer Center at Virginia Commonwealth University.
Josh Epworth: Hi, I'm Josh Epworth. I'm a nurse practitioner in hematologic malignancies at the University of Washington, Seattle Cancer Care Alliance in Seattle, Washington.
Sandy: In this video, we'll be discussing optimizing the use of current therapy options for relapsed or recurrent multiple myeloma as outlined in the learning objectives.
Sandy: So our focus today is on relapsed/refractory multiple myeloma. We know, though, that they are a changing paradigm. We know that in newly diagnosed multiple myeloma that that's very well defined. People are generally treated with a triplet regimen using a proteasome inhibitor and immunomodulatory agent and dexamethasone. We know that anti-CD38 antibodies and SLAMF7 antibodies are moving forward in that treatment paradigm, but we also know that multiple myeloma remains an incurable disease and that relapse is inevitable for the majority of patients.
Sandy: So framing our reference toward relapsed/refractory multiple myeloma, we know that the ISS staging for multiple myeloma has been recently revised, adding in lactate dehydrogenase, or LDH, and looking at beta-2-microglobulin levels, albumin in the old staging criteria, and then also adding in FISH analysis for selected cytogenetic abnormalities, particularly those that are considered to be high risk, such as 17p and translocation (4;14).
Sandy: So we're going to talk today specifically about how relapsed/refractory multiple myeloma is moving forward, and in order to really talk about relapsed/refractory multiple myeloma, we need to understand the definitions for progression of disease. We need to talk about what is stable disease, also depth of response. We're going to focus on undetectable minimal residual disease, or MRD, a little bit later. So let's talk first about biochemical versus clinical relapse. So Josh, talk to me a little bit about how you analyze that in your practice.
Josh: Well, when we're talking about a biochemical relapse, we're talking about a progression of numbers that were discovered later on in treatment of disease, where we find use of... increase of SPEP over a certain level, typically about 0.5 over the lowest... the nadir that we achieved. Or you can see if you don't have that opportunity, you can use UPEP, where you're seeing above 200 on that. Now, if you don't have the option to go with either UPEP or an SPEP, a free light chain ratio of greater than 10:1 is a usable approach.
Josh: We could also be looking at the production or growth of a neurolytic lesion or plasmacytoma. When we're talking about an actual clinical relapse, we're looking at really a recurrence of CRAB criteria where we're seeing these early biochemical markers begin to have an effect on organ systems in the body.
Sandy: Great. So the CRAB criteria being calcium, anemia, renal dysfunction, or detect for bone lesions, so you're basically having end organ damage, to your point. So then, we've more recently moved into this whole era of minimal residual disease testing and achieving that ultimate depth of response, where that is undetectable. So, Kevin, can you talk a little bit about how you're applying MRD in your clinical practice?
Kevin: Right. I think minimal residual disease has really become the standard when we think about treating patients on clinical trial. I think, in the setting of where we treat patients or where they're treated in the community, it's not one of those things that we actually look at and base treatment decisions upon. Very often, we think about patients being MRD negative at the end of, let's say, a transplant or prior to going on to maintenance therapy, and we can follow that at certain intervals, but we wouldn't make an actual treatment decision based upon recurrence of MRD. We would rather rate what like Josh was saying, more the traditional serum protein electrophoresis or serum free light chains.
Sandy: So let's then talk a little bit about the relapsed/refractory setting. We know that the standard of care in a newly diagnosed patient remains a triplet, generally a proteasome inhibitor, immunomodulatory agent, dexamethasone. We may see the monoclonal antibodies moving into that setting very soon, so we'd have a quad if you will. And then for most patients, transplant is still a standard of care and then followed by maintenance, and the most common maintenance therapy is lenalidomide as an immunomodulatory agent. So in those patients who progress after frontline therapy, talk to me a little bit about what your criteria is to treat these patients. Josh, we'll start with you.
Josh: Well, there are a host of issues that you have to address. One is, what's the most effective therapy that they can tolerate, what are their treatment options that we have, can we initiate another transplant if they've had one or if they're waiting for first relapse, if that's an option? Others are, what are their preferences? What's their accessibility to infusion settings? And can they afford some of the high-cost oral agents that are present now?
Sandy: Great, and, Kevin, anything to add to that?
Kevin: In addition, thinking about what they've had in terms of any residual side effects that remain and that's really an important one as well. And looking once again at performance status and if they're an older person, what their fragility score may be then as well. So re-establishing those points.
Sandy: So that is great. Now let's talk a little bit about the guidelines or the standards that are currently available to us to help guide the treatment decision-making in relapsed/refractory multiple myeloma. We know that many people use the National Comprehensive Cancer Network, the NCCN, guidelines. We know that those are important to guide reimbursement decisions, in addition to the Medicare compendia. We also know that we have mSMART. We know that there are guidelines put out for certain things by the International Myeloma Foundation, and more recently ASCO has partnered with clinical experts to put forth some guidelines for treatment. So talk a little bit about how you used those guidelines in deciding on how best to treat a relapsed/refractory multiple myeloma patient. Kevin, I'll start with you.
Kevin: Yeah, I think those guidelines are really important whether, which organization regardless, they're all very, very similar but not the same, and I think the important part of that is to, when we think about treating patients with different regimens, to know that there is at least some science behind those, if we decide to put a couple of different agents together in combination, that we can look at those guidelines and say, "Is this a good idea?” We can see data for those things as well. So guiding the treatment, in terms of those combinations is really important
Sandy: Let's talk a little bit more about how those guidelines tell us or don't tell us how to sequence therapy. Josh, I know that's a challenge in my practice.
Josh: It certainly is. We're all looking for the algorithm that can guide us through the best possible response with all these patients, and there really isn't one. There are studies that show a host of different outcomes based off of which medications to use. That said, as Kevin was mentioning, a lot of these guidelines have a lot of overlap. There are subtle differences between the 2 but we do always know that we're going to want to reach for a triplet therapy, which is our best option for getting the deepest next remission that we can possibly get. Where we choose from, are we going to initiate another proteasome inhibitor, another immunomodulator with steroids, or do we reach out to some of the more, the newer medications like a monoclonal antibody or other more advanced medications or studies?
Sandy: Great. So we're going to go a little bit further using some case studies to delve a little bit deeper into some examples of how you might use these guidelines and consider the different mechanisms of action of these agents and treatment decision making for multiple myeloma patients. So our first case is a relapsed patient after frontline therapy—so much of what we just talked about. But in this case, this patient was considered to be non–transplant eligible primarily due to age, so 75, and preference. There are some centers that will do autologous transplants in people that are 75 and in good health, but this patient has chosen not to proceed with that.
Sandy: According to the standard of care, she received a triplet regimen proteasome inhibitor, immunomodulatory drug and dexamethasone and achieved a very good partial response, which we know is, in most centers, a criteria to move forward to transplant still today, but discontinued treatment 9 months after completing those cycles, primarily due to progressive neuropathy, so side effects.
Sandy: She's now being followed and she's having 3 or 4 incremental increases in serum free light chains. And so talk to me a little bit about your approach to this patient who now is going to be 76 years old, who's showing these incremental increases. So Kevin, how would you go forward with this?
Kevin: I think, first and foremost, the thing to think about is she's having a biochemical relapse. So this is not something rapid, and we have time to make a decision and present some options to her. So I think that's first and foremost; we don't have to jump into it. I think secondly we look at what does she have previously? And she did have the standard with bortezomib, lenalidomide, and dexamethasone, but she had some issues with that, which was neuropathy, and she got a very good partial response, that's nice, and we could even think about going back to that. But with the neuropathy, we have to think that might not be a good idea, and then we move on to something else.
Kevin: I think the other thing to look at, I believe she was an intermediate fit and had pretty good performance status when she was first diagnosed, but this is 2 years later. We do know her husband passed away in the interim and things like that. So again, re-establishing how, if she's still at intermediate fit, and then how has her social situation changed or financial situation with her husband dying as well. So a couple of those things we'll take into consideration.
Sandy: So a lot of the real-life factors play a huge role in this.
Kevin: Correct.
Sandy: We know there are a number of trials that have been recently reported for the relapsed/refractory setting in general and in every case, triplets outdid doublets. So again, adding 3 drugs from different mechanisms of action, including those that added a monoclonal antibody or a SLAMF7 antibody such as elotuzumab, the anti-CD38 antibody of daratumumab to a doublet was far superior in most cases, in every element, progression-free survival, duration of response, time to response, and depth of response, in those studies.
Sandy: So talk to me a little bit about this kind of patient, looking at introducing one of these triplet regimens in with pre-existing neuropathy and who's already been exposed to several of those categories of drugs. So Josh, well, how would you approach that?
Josh: Well, I think Kevin brought up a lot of great points of what we need to be thinking about when we start a treatment or decide on a treatment, but one of the things in going forward with this patient is that we don't know what her cytogenetics are at this point. She might have mutated into a high-risk disease, which is going to significantly change when we start treatment and with what. If we're seeing as a high-risk disease, in particular, 17p deletion, it's always going to guide us towards a proteasome inhibitor.
Josh: In this case, as Kevin mentioned, that because of the peripheral neuropathy and the occurrence of peripheral neuropathy with bortezomib, we might be wanting to reach for something like carfilzomib if we are content with her cardiac status or we are content that she's not going to have any respiratory issues, so that's going to guide us in one part. This patient has had lenalidomide in the past and she's tolerated it well, and there's an argument to be stated that, well, it's been effective and well tolerated that it can be utilized again. In addition, even if she had been on maintenance lenalidomide, there is an argument to be stated that she could go on treatment levels of lenalidomide because we haven't seen it at those levels when in combination with a triplet therapy.
Josh: However, it does have side effects, so we may want to consider going to the next immunomodulator like pomalidomide. Another thing that we need to think about in coming up with this combination is, this is an older woman, how is she going to tolerate the steroid levels? We have to be conscious of all 3 medications that we're introducing to her.
Sandy: So that's a really important point, is considering any residual adverse events from prior therapies and then the other, I think key thing that you've brought up is the fact that if you have progressed on a drug that is in a certain class based on mechanism of action, an immunomodulatory agent, for instance, lenalidomide, most of these trials have also validated that you can still respond to a drug in that same class. So in this case, pomalidomide being an immunomodulatory agent.
Sandy: People can respond to that drug, where they've been refractory to a prior drug in the same class. So another very important factor. You talk a little bit about pulmonary/cardiovascular toxicity; what are the other adverse events that you've seen where you have to really consider that in terms of what you're going to do next?
Kevin: Right. I think, like with all of our medications, the GI side effects can be pretty significant in patients, and so managing those is really important, and predominantly we'll see a lot of issues with diarrhea, and when we think about a 77 year old and we think about dehydration and that type of thing. Fortunately, nurses have been very good at managing diarrhea over the years and other GI side effects and so... But each drug is going to have its particular side effects, some less than others, and sometimes that just might guide us to another medication as well.
Kevin: Again, we're looking at those different mechanisms of action, and the nice thing we have is a variety of drugs in each class of a couple of proteasome inhibitors, a couple of immunomodulatory agents, and a couple of monoclonal antibodies. So if we think about the side effects they were having that maybe we didn't get much control on, we could move to another drug in the same class that worked well.
Sandy: Great. So let's now move to the second case. So this is a younger patient, 58 years old, stage III based on the revised ISS criteria, IgG lambda, and has a translocation (4;14). So that's a specific problem. Typical RVD induction, followed by a very good partial response, goes to transplant, maintenance lenalidomide. After 4 months post-transplant, this patient has a rising M protein, his kappa/lambda ratio is rising, he's developed severe back pain, which on PET imaging shows a paraspinal plasmacytoma. So he's relapsed very soon after his initial treatment, knowing that this is basically high-risk disease now. He also developed insulin-dependent diabetes, which we know can be an issue with this steroid exposure and his ejection fraction has now dropped to 45%.
Sandy: So talk to me a little bit about... We know there is also no role for tandem transplants in this population because we know that soon after transplant, that's not effective. We know there are a number of studies that have looked at how to approach this therapy with these patients, early versus late relapse. So this is... Let's focus on the early relapse. Talk to me about how you would approach this patient, Josh, in selecting the next line of therapy.
Josh: He's in a complicated position because he's young. He's had an early relapse, he has multiple high-risk factors that are present. In addition to that, we have some issues with what medications we can choose with the pulmonary issues, the reduced... the cardiac issues with the reduced ejection fraction that may make a problem if we're reaching for carfilzomib as a medication. In addition, we again have to be cautious with our use of steroids in a person with diabetes.
Josh: In this case, I guess I would consult. First thing would be to consult with cardiology to see if this was a safe approach and we're very fortunate in the center I work in, where we have cardiologists who are both aware of the study of the heart but also how it affects in the setting of oncology. If that was a possibility, carfilzomib is a reasonable choice. Daratumumab is also a reasonable choice. In addition, we can combine that with pomalidomide and a reduced-dose steroid or closely monitored steroids.
Josh: Great. Kevin, would you approach it in any different way?
Kevin: No, I think Josh hit the numbers absolutely perfect. This happens a lot, high-risk cytogenetics and a rapid relapse while on a doublet, and so we do have to reach into the bag and find something that's going to be really effective for this guy, and he's, unlike the first case, this person needs to be treated right away as he now has those CRAB criteria.
Sandy: Right. And he's got a paraspinal mass.
Kevin: Absolutely.
Sandy: And so talk to me a little bit about... do you include ever radiation in these patients who have masses around a paraspinal mass versus elsewhere?
Kevin: Yes, we do. Very often, we do. Especially a paraspinal mass because we worry about vertebral problems and cord compression and things like that. With some other lesions, we're not necessarily going to radiate those. We don't like to spot weld patients as it is, and the systemic treatment will generally take care of those and actually fairly rapidly when they respond.
Sandy: Great. And so let's talk a little bit more about interdisciplinary management as advanced practitioners and how do you reach out to your colleagues and other specialties. I think we talked about the cardiologist or onco-cardiologist, which is now a thing where these... We're grateful that these cardiologists have really focused in the area of oncology but in this patient, we might also wat to get an endocrinologist to help us manage that diabetes. Are there other things that you might do in terms of interdisciplinary management for this patient?
Kevin: Yeah, I think so. We have very good supportive care clinic as well, and a majority of our patients will actually be introduced to that group as well and they do anything from psychosocial issues to financial issues to pain issues and to get them on board as well. We do have the benefit of an endocrinologist who works just with our oncology patients as well. So that's a huge benefit much like the cardiology, which you have as well, and so anybody we can bring in to manage those. And again we think about this guy, if he's having a rapid relapse to get those things under control from a cardiology standpoint, an endocrine standpoint really important for that next line of treatment.
Sandy: Now let's think if this patient relapsed 3 years after transplant while on maintenance. We know that maintenance therapy is the standard of care today, and we know that there's some lack of clarity on how long that lasts, maintenance therapy, but let's say this patient relapses 3 years after this transplant. Josh, how would you approach that differently?
Josh: It gives us another option in the sense that we can reach out and use another auto stem cell transplant if he's amenable. The minimum that we like to see is about 3 years because we make an assumption that the second transplant is going to be half as effective, meaning 18 months as the first transplant. So we'd want to have a long conversation with him about the benefits of doing a transplant but also his expectations of what he would get out of this. We don't want him going into this situation thinking he's going to definitely get another 3 years. We cannot guarantee that.
Sandy: Great. And you would need to talk about what to do to get there, right? Because we need them to be at least a VGPR prior to transfer. We know that patients that are less than that in terms of depth of response do not do as well. So, what might you consider? You've consulted cardiology, you've got endocrine on board, you've got him tuned up, if you will, in terms of his residual comorbidities from prior therapy. What kinds of considerations would you have given that this patient had RVD auto transplant lenalidomide maintenance?
Kevin: Right. So I think the difference between this and the first scenario and this gentleman is in the first scenario, he relapsed on doublet therapy, which included a proteasome inhibitor. In this situation, he didn't. So we have, potentially we can go back to that original proteasome inhibitor because that in combination with the transplant seemed to do a pretty good job. So I think we could do that. That gives us one option, rather than changing proteasome inhibitors and again, if we got this guy tuned up over a period of time of 3 years, I think the risk for carfilzomib is potentially a little bit less and so that helps us as well. Hopefully, we've got his endocrine issues taken care of as well. So it opens up our pathway, opens up the bag a little bit more to reach in for different and a more diverse group of triplet regiments to try on him.
Sandy: So really what we are talking about in this scenario is the variability in approach to treatment in these patients with relapsed/refractory multiple myeloma. Even with the guidelines, much of this comes down to clinical expertise of the team, the advanced practitioner and physicians that are taking care of these patients and really knowing that patient as an individual in both their disease state and social situation and selecting the best therapy for those patients.
Sandy: Thank you for joining us for this activity.
Sandy: We're going to talk about PEARLs or a recap of key points and strategies for practice application. These include risk-adapted treatment selection, considering age, fitness, disease profile, risk category, the use of triplet regiments including a immunomodulatory agent, proteasome inhibitor, and dexamethasone plus or minus a monoclonal antibody, yet we know preferred sequencing remains unclear. Standards for evaluating response, including minimal residual disease status, are evolving. What can you do? Regularly participate in continuing education activities to stay abreast of the rapidly evolving science, relative to relapsed/refractory multiple myeloma, apply your understanding of the mechanism of action of each agent used to treat relapsed/refractory multiple myeloma in treatment selection and sequencing, and incorporate strategies or processes for the assessment of frailty and comorbidities to tailor treatment decision making and adverse event mitigation and management. Know that minimal residual disease remains investigational in the relapsed/refractory multiple myeloma setting.
Sandy: Thank you for joining us.
These activities, certified for CME/CE/CPE credit, are jointly provided by
  |
From Quandary to Clarity in Relapsed/Refractory Multiple Myeloma: Optimizing Treatment and Empowering Patients
Activity 1: Therapy for Relapsed/Refractory Multiple Myeloma (RRMM)–Optimizing Use of Current Options
Multiple myeloma (MM), a hematologic malignancy plagued by multiple relapses, has seen notable progress in care that has led to improved survival. Contributing to the progress has been an increased understanding of MM pathogenesis and cytogenetics-based risk stratification and the availability of therapeutics such as immunomodulatory drugs, proteasome inhibitors, and novel targeted therapies. Keeping up with these advances is especially challenging for community-based clinicians for whom MM may represent only a small fraction of their total patient population.
With the continued rapid pace of advances in MM, management of patients with relapsed/ refractory (RR) disease is becoming increasingly complex and requires careful evaluation and interpretation of new and emerging data. To help advanced practitioners (APs) enhance their roles as educators and advocates, strategies for effectively educating patients and engaging them in shared decision making are also needed.
From Quandary to Clarity in Relapsed/Refractory Multiple Myeloma: Optimizing Treatment and Empowering Patients is an educational initiative designed to improve the ability of APs to provide high-quality care for patients with RRMM. This initiative includes:
- 3 expert clinical dialogues (video-based activities) certified for continuing education credit
- Downloadable resources including transcripts and slides for each of the certified activities and links to related guidelines, articles, and websites
- Downloadable patient education materials
Release date: 07/31/2019
Expiration date: 07/31/2020
Estimated time to complete: 30 minutes
Fee: None
This activity is designed to help clinicians achieve specific learning objectives, which reflect the desired results of the education. Participants are encouraged to integrate what they learn from this activity into practice to improve patient care and outcomes.
Jointly provided by
Faculty
Sandra Kurtin, PhD, ANP-C, AOCN®
Kevin Brigle, PhD, ANP
Josh Epworth, MSN, ARNP
Intended Participants
This activity is designed for community-based advanced practitioners (eg, nurse practitioners, advanced practice nurses, physician assistants, oncology pharmacists) who provide care for patients with RRMM. Those practicing in academic and comprehensive cancer centers may also choose to participate.
Learning Objectives
After completing this activity, clinicians should be better able to:
- Relate the mechanism of action of current and/or emerging therapies for RRMM to their expected and proven therapeutic effects and toxicities
- Interpret the clinical significance of findings from clinical trials supporting the efficacy and safety of approved and/or emerging therapeutic regimens and strategies for RRMM
- Plan strategies for selecting and sequencing therapy for patients with RRMM
- Identify potential adverse events associated with approved and/or novel agents used to treat RRMM
- Devise strategies for mitigating adverse events associated with therapies for RRMM
Continuing Education
Certification
This activity is certified for credit by Annenberg Center for Health Sciences at Eisenhower.
39000 Bob Hope Drive, Dinah Shore Building, Rancho Mirage, CA 92270
Voice: 760-773-4500; Fax: 760-773-4513; E-mail: contactce@annenberg.net
© 2019, Annenberg Center for Health Sciences at Eisenhower. All rights reserved.
Statement of Credit
Participants who successfully complete this activity—which includes submitting a completed pre-test, submitting and scoring at least 70% on the post-test, and submitting a completed evaluation form—will be able to download a statement of credit.
To access the learning assessment and evaluation form, visit https://education.annenberg.net/5741-1
Accreditation and Designation Statements

Physicians. This activity has been planned and implemented in accordance with the accreditation requirements and policies of the Accreditation Council for Continuing Medical Education through the joint providership of the Annenberg Center for Health Sciences at Eisenhower and Harborside Medical Education. The Annenberg Center is accredited by the ACCME to provide continuing medical education for physicians.
The Annenberg Center for Health Sciences at Eisenhower designates this enduring activity for a maximum of 0.5 AMA PRA Category 1 Credits™. Physicians should claim only the credit commensurate with the extent of their participation in the activity.

Nurses. Annenberg Center for Health Sciences at Eisenhower is accredited as a provider of continuing nursing education by the American Nurses Credentialing Center’s Commission on Accreditation.
A maximum of 0.5 contact hour may be earned for successful completion of this activity.
Provider is approved by the California Board of Registered Nursing, Provider No. 13664, for 0.5 contact hour.

Pharmacists.
The Annenberg Center for Health Sciences at Eisenhower is accredited by the Accreditation Council for Pharmacy Education (ACPE) as a provider of continuing pharmacy education. This activity has been assigned ACPE Universal Program #0797-9999-19-064-H01-P. This activity is designated for up to 0.5 contact hour (0.05 CEU) of continuing pharmacy education credit. This is a knowledge-based activity.
Disclosures
Commercial Support
This activity is supported by educational grants from AbbVie Inc. and Celgene Corporation.
Relationships of Faculty and Planners
All individuals in a position to control the content of this activity (eg, planners, faculty, reviewers) must disclose all financial relationships with commercial interests that may have a bearing on its subject matter. The Annenberg Center for Health Sciences at Eisenhower has identified and resolved all conflicts of interest in accordance with its policies and procedures. Participants should assess the impact (if any) of the disclosed information on the educational value of the activity.
Faculty
Sandra Kurtin, PhD, ANP-C, AOCN®, is a consultant for AbbVie, Acceleron, Amgen, Celgene, Genentech, Incyte, Novartis, and Pharmacyclics.
Kevin Brigle, PhD, ANP, is on the speakers bureau for Amgen, AstraZeneca, Celgene, Genentech, Novartis, and Takeda.
Josh Epworth, MSN, ARNP, has nothing to disclose.
Planners and Reviewers
Staff of and consultants for the Annenberg Center for Health Sciences at Eisenhower and Harborside Medical Education have nothing to disclose.
Product Disclosure
This activity may include discussion of agents that have not yet been approved by the U.S. Food and Drug Administration and investigational uses of approved products. Please consult prescribing information and practice guidelines for detail regarding safe and effective use of therapeutic agents.
Disclaimer
The opinions expressed in this activity are those of the faculty and do not represent an endorsement by Annenberg Center for Health Sciences at Eisenhower of any therapeutic agent or approach to diagnosis or patient management.